Healthcare financial management: A comprehensive guide

- Healthcare financial management fundamentals
- Revenue cycle management: The financial backbone
- Healthcare budgeting and financial planning
- Financial reporting and analysis in healthcare
- Cost management strategies
- Technology and innovation in healthcare finance
- Future trends and best practices
- Streamline healthcare financial management with Ramp
Healthcare financial management helps healthcare organizations stay financially stable so they can focus on what matters most: delivering quality patient care. In an industry shaped by rising costs, changing regulations, and complex reimbursement models, effective financial management gives you the structure to plan for growth, manage risk, and keep resources aligned with mission and care goals.
Healthcare financial management fundamentals
Healthcare financial management is the strategic planning and day-to-day control of a healthcare organization’s finances while delivering effective patient care. Its scope includes budgeting and forecasting, revenue cycle management, cost controls, capital investments, risk management, regulatory compliance, and reporting and audits.
Key objectives include maximizing revenue, controlling costs, ensuring compliance, managing financial risk, improving efficiency with technology, and supporting long-term sustainability.
The 4 Cs Framework
The 4 C’s of healthcare finance—cost, cash, capital, and control—provide the foundation for sound financial management. Each helps healthcare leaders balance patient care with fiscal responsibility.
- Cost: Manage spending across labor, supplies, and overhead while maintaining patient care standards. Look for savings through vendor negotiation, waste reduction, and better use of resources.
- Cash: Keep liquidity steady to meet daily obligations and fund growth. Strong cash flow management shortens payment cycles and reduces days in accounts receivable.
- Capital: Plan and prioritize long-term investments (e.g., new facilities or technology) based on financial return and impact on care quality
- Control: Maintain oversight through clear policies, internal audits, and compliance checks to prevent errors and protect assets
The role of healthcare financial managers
Healthcare financial managers play a central role in maintaining an organization’s financial health. They analyze performance metrics, manage reimbursements, and implement financial controls to prevent inefficiencies and fraud. Day to day, they oversee budgeting and forecasting, review capital plans, and ensure compliance with healthcare regulations and reporting standards.
The work is collaborative. Financial leaders partner with department heads, clinicians, and executives to align spending with strategic priorities and maintain accountability across the organization. They also work with external stakeholders such as insurers, auditors, and regulators to support accurate reimbursement and transparency.
Common roles within healthcare finance include:
- Chief financial officer (CFO): Oversees overall financial strategy, manages risk, and ensures long-term stability
- Financial analyst: Evaluates data and trends to guide budgeting and investment decisions
- Revenue cycle manager: Oversees billing, coding, and collections to improve cash flow and minimize claim denials
- Budget analyst: Develops and monitors budgets to ensure resources are allocated efficiently
- Compliance officer: Ensures adherence to financial and healthcare regulations through audits and internal policies
Revenue cycle management: The financial backbone
Revenue cycle management (RCM) connects the care a provider delivers to the payment it receives. It covers every step from patient registration through final reimbursement—and it’s what keeps cash flowing, compliance intact, and operations sustainable. Strong RCM helps reduce claim denials, improve collection rates, and shorten payment cycles.
The complete revenue cycle process
- Patient registration and insurance verification: Capture patient and insurance details, confirm eligibility, and collect co-pays and deductibles
- Medical coding and charge capture: Translate clinical documentation into accurate billing codes that support medical necessity
- Claims submission and processing: Format and send claims according to payer rules; track for acceptance or rejection
- Payment posting and reconciliation: Record payments, match them to claims, and flag underpayments or discrepancies
- Denial management and appeals: Identify root causes of denials, correct issues, and manage appeals quickly
- Patient billing and collections: Communicate clearly, offer payment plans and digital options, and reduce outstanding balances
Industry benchmarks suggest average denial rates hover around 5–10%, with best-performing systems closer to 3%, according to MD Clarity.
Common RCM challenges and solutions
- Human error and coding mistakes: Invest in staff training and regular internal audits to catch and prevent issues early
- Constant regulatory change: Designate a compliance lead to monitor payer and policy updates
- Technology silos: Integrate EHR, billing, and clearinghouse systems for smoother data flow
- Patient payment delays: Offer transparent pricing, digital payment options, and card-on-file programs to encourage timely payments
- Limited visibility: Use RCM dashboards and analytics tools to track key performance indicators (KPIs) in real time
Key RCM performance metrics
| KPI | What it measures | Typical benchmark |
|---|---|---|
| Net collection rate | Cash collected vs. collectible A/R | 95%–99% |
| Days in accounts receivable | Time to collect payment | 30–45 days |
| First-pass claim rate | Claims paid without rework | 85%–95% |
| Denial rate | Percentage of claims denied | <5% |
| Cost to collect | Cost per $1 collected | $0.03–$0.05 |
Healthcare budgeting and financial planning
There are many unique challenges to healthcare budgeting that you don’t find in other industries because of the highly regulated and service-oriented nature of the industry. Some of the challenges include:
- High fixed costs
- Unpredictable patient demand
- Diverse payer mix (including self-pay, insurers, Medicare, and Medicaid)
- Regulatory compliance
This is why it’s crucial to align budgets and financial plans with your organization’s strategic goals. Always keep your mission in mind to ensure your resources support the best possible care, that capital investments align with growth planning, and staffing plans represent evolving care models and population health needs. Most importantly, your measurable financial goals need to be sustainable for your organization’s real operations.
Types of healthcare budgets
Healthcare budgeting must balance financial discipline with mission-driven care. Unlike other industries, healthcare faces high fixed costs, unpredictable demand, complex payer mixes, and constant regulatory change. Strong financial planning aligns limited resources with strategic goals and ensures the organization can grow sustainably while maintaining quality care.
- Operating budget vs. capital budget: Operating budgets track day-to-day revenue and expenses like payroll or supplies. Capital budgets are different in that they fund long-term investments such as new equipment, facilities, or technology upgrades.
- Incremental budgeting: Builds on last year’s budget with small adjustments. It’s simple but can carry forward inefficiencies if not reviewed.
- Zero-based budgeting: Starts from scratch each year and requires justification for every expense. Useful for resetting spend but resource-intensive
- Activity-based budgeting: Ties costs to activities or service volumes, improving transparency by linking financial goals to operations
- Rolling forecasts: Continuously update the budget to reflect new information, which is ideal for dynamic payer environments and variable patient volumes
Budgeting methods at a glance
| Method | When to use | Watch-outs |
|---|---|---|
| Incremental | Stable operations | May preserve inefficiencies |
| Zero-based | Reset or reprioritize spending | Labor-intensive to execute |
| Activity-based | Service-line transparency | Needs accurate activity data |
| Rolling forecast | Volatile volumes or rates | Requires disciplined cadence |
Budget development process
A structured process ensures financial plans reflect strategy and reality.
- Data collection and historical analysis: Review prior-year volumes, revenue, and costs to identify trends and anomalies
- Volume forecasting and revenue projections: Model changes by service line, payer mix, and reimbursement rates
- Expense planning and resource allocation: Align staffing, technology, and supply costs with strategic priorities
- Stakeholder involvement and buy-in: Engage executives, clinicians, and department leads to align goals and secure accountability
Many organizations also use rolling forecasts, updated monthly with a 12–18-month outlook, and set variance thresholds (for example, ±3%) that prompt review and corrective action.
Managing budget challenges
Healthcare budgets are never static. These are common challenges and ways to address them:
- Unpredictable patient volumes: Use real-time analytics and rolling forecasts to respond quickly to change
- Fragmented payer environment: Optimize contracts and revenue cycle processes to improve predictability
- Rising labor and supply costs: Plan for inflation and shortages; consider group purchasing and automation to control expenses
- Regulatory compliance costs: Build reporting and quality mandates into budgets and streamline workflows through technology
Financial reporting and analysis in healthcare
Accurate financial reporting is the foundation of sound decision-making in healthcare. It helps leaders allocate resources, plan strategically, and stay compliant with standards from agencies such as the Centers for Medicare & Medicaid Services, the Affordable Care Act, and HIPAA.
Essential financial reports
Healthcare financial managers rely on a few core reports to track performance and maintain compliance:
- Income statement: Shows revenue, expenses, and profit or loss over time to gauge financial performance
- Balance sheet: Provides a snapshot of assets, liabilities, and equity to evaluate financial stability
- Cash flow statement: Tracks inflows and outflows to assess liquidity and support short-term planning
Key performance indicators (KPIs)
KPIs provide ongoing visibility into financial health and operational efficiency. Common metrics include:
- Operating margin
- Revenue per patient
- Denial rate of claims
- Days in accounts receivable (A/R)
- Cost to collect from patients
- Net collection rate
- Clean claim rate
Tracking these metrics regularly helps teams identify trends, improve billing accuracy, and strengthen cash flow.
Financial analysis techniques
Financial analysis helps healthcare organizations understand their numbers and make data-driven choices.
- Trend analysis: Identify shifts in volume, cost, or revenue over time
- Ratio analysis: Measure liquidity and profitability using balance sheet and income statement data
- Variance analysis: Compare actual results against budget expectations to highlight drivers of change
- Benchmarking: Compare KPIs to industry averages to spot opportunities for improvement
Cost management strategies
Healthcare cost management means finding ways to control spending without sacrificing quality care. It’s an increasingly urgent priority: the Centers for Medicare & Medicaid Services projects that U.S. healthcare spending will grow by about 5.8% per year through 2033, outpacing the economy. Managing those costs is essential to long-term sustainability and patient access.
Common cost-control approaches include investing in preventive care, standardizing clinical protocols, renegotiating payer contracts, and reducing operational waste. The goal is balance: every efficiency should support better patient outcomes, not compromise them.
Direct and indirect cost management
Cost management falls into two interconnected categories: direct costs (related to patient care) and indirect costs (supporting services and administrative overhead). Here are some of the ways to approach both types of costs:
Labor cost optimization
At many organizations, labor is the greatest expense. You can keep your labor costs under control by using:
- Flexible staffing models and per diem staff to keep costs down
- Productivity tracking for clinical and non-clinical staff against KPIs
- Task delegation toward the greater care team (including NPs and residents) to keep quality high, but costs low
Supply chain management
When individual departments or service lines are making their own purchases, it can lead to waste and inefficiencies. To reduce waste, work towards standardizing supplies and procedures across your organization and leverage group purchasing to secure better rates and negotiating power. Implement inventory tracking to ensure you have the necessary supplies on hand to care for patients.
Technology investments and ROI
Technology, when used correctly, can go a long way in driving efficiencies in cost management and improving quality. These tools are some of the most commonly used in healthcare:
- Electronic Health Record (EHR): Standardized EHR systems, like Epic and Oracle Health, improve coordination, consistency, and billing practices
- Virtual care and telehealth: Many ailments can be diagnosed initially during virtual or telehealth calls, which increases patient access and reduces the overhead of in-person visits
- AI and analytics tools: Modern healthcare organizations are using AI and similar tools to predict patient risk, reduce unnecessary interventions, and optimize scheduling and billing
Just remember, tools don’t automatically solve problems. You need to align technology with your strategic plans and evaluate your ROI based on cost controls and patient outcomes.
Outsourcing considerations
There are ways to outsource certain operations to reduce overhead. Outsourcing some of your indirect service costs can help with efficiencies, so long as they maintain your high level of quality service and compliance standards.
Consider outsourcing things like:
- Billing
- IT
- Laundry services
- Call centers
- Food services
Value-based care and cost management
Value-based care represents a shift from the traditional fee-for-service model, where providers are compensated for the services they deliver. In value-based care, the emphasis is on improving patient outcomes and rewarding providers for positive results.
The volume of procedures is no longer what’s celebrated, but rather the value of outcomes per dollar spent, the quality of care, and cost efficiency. This requires a new alignment of resources to meet these expectations across the evolving healthcare space.
Quality metrics and financial performance
With value-based care, success means meeting quality targets. These are some of the metrics that help define financial success:
- Patient satisfaction
- Readmission rates
- Infection rates
- Compliance with preventative care
By linking these types of metrics to financial incentives for providers, you can keep costs in check while driving improvements in care. But this means that providers are sharing in the fiscal responsibility and the risk that comes with it.
When providers meet their quality metrics, they can receive financial bonuses. However, when they don’t, there could be penalties. Because these kinds of arrangements can be complex, you need robust care coordination and data infrastructure to support.
Technology and innovation in healthcare finance
New technologies continue to transform both healthcare delivery and financial management. Modern healthcare organizations use automation, analytics, and AI to streamline operations, reduce manual work, and improve accuracy across billing, budgeting, and forecasting. These tools give finance teams a clearer view of performance, allowing them to make faster, data-driven decisions.
Automation and AI applications
Automation and artificial intelligence are playing an increasingly central role in healthcare finance. Robotic process automation (RPA) now handles repetitive tasks like charge capture and coding validation, while natural language processing (NLP) can extract billing details directly from physician notes. Predictive analytics helps forecast revenue and patient volumes, identify risks in payer mix, and improve resource allocation.
AI-driven denial management tools are also becoming more common. Since 2020, according to data from Kodiak Solutions, denied claims have increased by more than 16%, and AI helps organizations get ahead of those issues by identifying patterns early and even generating appeal drafts. Real-time dashboards bring everything together, integrating KPIs across departments so leaders can make adjustments before small issues become big problems.
Integration and interoperability
New technology systems don’t exist in a vacuum. They’re only ever as good as the integrations they support both clinically and operationally. These are the key integration considerations:
EHR and financial system integration
Building a link between your EHR and financial system ensures unified data flow. When charges and codes are captured, they flow accurately and seamlessly into your billing systems. Automating the process means fewer errors from data entry and re-entry as the data moves from the clinical to the finance team.
Data governance and quality
Your data governance best practices are a cornerstone of transparency and accountability. Utilizing Master Data Management (MDM) processes ensures your data is accurate and consistent across your various systems. When your key metrics remain consistent within your organization, there’s less confusion and fewer mistakes in claims.
Cybersecurity considerations
Healthcare systems are frequent targets of cybersecurity threats. The average cost of a cyberbreach of healthcare data is nearly $10 million.
Sensitive information such as patient data, financial records, and insurance details is protected under HIPAA and other regulations. Non-compliance can disrupt your operations or lead to legal and financial trouble. Make sure to keep your access controls buttoned up, utilizing multi-factor authorization and role-based access to data.
Future trends and best practices
Healthcare financial management continues to evolve as regulations tighten, costs rise, and technology advances. To stay competitive, be ready to adapt your financial strategies and workforce to meet new challenges while maintaining a focus on quality and transparency.
Value-based payment models
As healthcare shifts from a volume-based model to one centered on outcomes, reimbursement increasingly depends on efficiency, prevention, and patient satisfaction. Programs such as bundled payments, shared savings contracts, and risk-sharing agreements reward providers for improving care while reducing costs. To succeed, organizations must integrate financial and clinical data to measure performance and justify reimbursements accurately.
Patient-centered and consumer-driven healthcare
Patients are now active participants in their care decisions, often comparing costs and experiences before choosing a provider. Retail entrants and digital-first care models such as Amazon’s growing healthcare business are reshaping expectations for access and convenience. To compete, healthcare organizations should invest in self-service portals, online scheduling, and transparent billing tools that make healthcare as seamless as any consumer experience.
Price transparency requirements
Federal regulations now require hospitals and payers to share clear, consumer-friendly pricing information, including out-of-pocket costs and negotiated rates. Noncompliance can lead to penalties—and more importantly, erode patient trust. Providers that adopt digital tools for compliance and patient education will be better equipped to meet both regulatory and reputational demands.
Workforce planning and development
Workforce shortages remain one of healthcare’s most urgent financial pressures. The American Association of Colleges of Nursing projects that the shortage of registered nurses will continue to grow as demand rises and the workforce ages. You can plan for this shift by investing in analytics-driven workforce planning, cross-training programs, and competitive compensation and benefits to retain talent and maintain care quality.
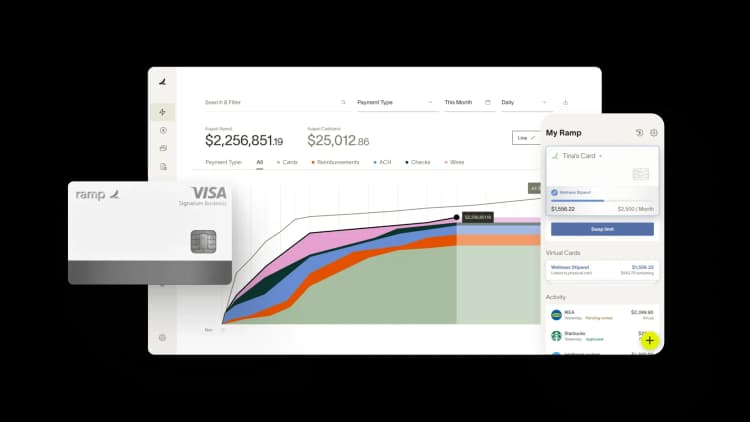
Streamline healthcare financial management with Ramp
Finance leaders are increasingly turning to Ramp, as managing the financial complexities of healthcare requires precision, agility, and the right tools to maintain profitability while delivering top-tier patient care. Ramp’s suite of products, including automated expense management, vendor payments, and powerful spend analysis, provides healthcare organizations with the visibility and control they need to thrive.
Automate your expense tracking and vendor payments, reducing the time spent on administrative tasks, and refocus your efforts on what matters most—improving patient outcomes. With Ramp’s real-time spend insights, your organization can optimize resource allocation, contain costs, and ensure financial stability. Simplify healthcare finance management today with Ramp’s finance solutions and see how your organization can save time and money.

FAQs
AP outsourcing is a solid choice when scaling quickly or lacking specialized staff. But modern AP software platforms can also deliver comparable efficiency gains without the ongoing outsourcing fees.
“In the public sector, every hour and every dollar belongs to the taxpayer. We can't afford to waste either. Ramp ensures we don't.”
Carly Ching
Finance Specialist, City of Ketchum

“Ramp gives us one structured intake, one set of guardrails, and clean data end‑to‑end— that’s how we save 20 hours/month and buy back days at close.”
David Eckstein
CFO, Vanta

“Ramp is the only vendor that can service all of our employees across the globe in one unified system. They handle multiple currencies seamlessly, integrate with all of our accounting systems, and thanks to their customizable card and policy controls, we're compliant worldwide. ”
Brandon Zell
Chief Accounting Officer, Notion

“When our teams need something, they usually need it right away. The more time we can save doing all those tedious tasks, the more time we can dedicate to supporting our student-athletes.”
Sarah Harris
Secretary, The University of Tennessee Athletics Foundation, Inc.

“Ramp had everything we were looking for, and even things we weren't looking for. The policy aspects, that's something I never even dreamed of that a purchasing card program could handle.”
Doug Volesky
Director of Finance, City of Mount Vernon

“Switching from Brex to Ramp wasn't just a platform swap—it was a strategic upgrade that aligned with our mission to be agile, efficient, and financially savvy.”
Lily Liu
CEO, Piñata

“With Ramp, everything lives in one place. You can click into a vendor and see every transaction, invoice, and contract. That didn't exist in Zip. It's made approvals much faster because decision-makers aren't chasing down information—they have it all at their fingertips.”
Ryan Williams
Manager, Contract and Vendor Management, Advisor360°

“The ability to create flexible parameters, such as allowing bookings up to 25% above market rate, has been really good for us. Plus, having all the information within the same platform is really valuable.”
Caroline Hill
Assistant Controller, Sana Benefits



