Sunshine Act compliance explained: Requirements, challenges, and solutions

- What is the Sunshine Act?
- Who needs to comply with Sunshine Act reporting requirements?
- What information must be tracked and reported for compliance under the law?
- Is manual Sunshine Act compliance challenging for finance teams?
- Where automation fits in Sunshine Act compliance workflows
- Which expenses benefit most from compliance automation
- What makes automation the foundation for Sunshine Act compliance?
- Where Ramp fits in your Sunshine Act compliance process
The Sunshine Act requires life sciences companies to report payments and transfers of value made to physicians and teaching hospitals. Each transaction needs to be documented and submitted with precision.
The challenge isn’t understanding the law. It’s managing the complexity of compliance. Data often sits in multiple systems, and manual reconciliation makes it difficult to ensure accuracy. Automation changes how you manage this requirement. By centralizing spend data and applying consistent rules, compliance becomes faster and more reliable.
What is the Sunshine Act?
The Sunshine Act is a U.S. federal law that requires manufacturers of drugs, medical devices, and biologics to report payments and other transfers of value made to physicians and teaching hospitals. The law was introduced in 2010 as part of the Affordable Care Act and is also known as the Open Payments Program.
Under the Sunshine Act, you are required to submit annual reports to the Centers for Medicare & Medicaid Services (CMS). These reports capture both direct payments, such as consulting fees and research funding, and indirect transfers, including meals, travel, and educational materials. In 2024, CMS reported more than 16.16 million records with a combined value of over $13.18 billion.
The goal is transparency. By making financial relationships between healthcare providers and life sciences companies public, regulators aim to reduce conflicts of interest and strengthen patient trust. You gain clarity on what must be reported. But the obligation to track and document each payment rests with your finance and compliance teams.
Who needs to comply with Sunshine Act reporting requirements?
The Sunshine Act places reporting responsibility on organizations that manufacture, distribute, or arrange for the purchase of covered drugs, devices, biologics, and medical supplies, ensuring regulatory compliance. Compliance is not limited to manufacturers alone. It spans the ecosystem of life sciences companies that shape how products reach healthcare providers.
You fall under the reporting rules if your company fits into one of the following categories:
- Applicable manufacturers: Producers of drugs, devices, biologics, or supplies reimbursable by Medicare, Medicaid, or CHIP. Reporting applies whether the product is marketed in the U.S. directly or through affiliates.
- Entities under common ownership: Subsidiaries or sister companies that assist with the manufacturing, marketing, promotion, or distribution of covered products. Even if they do not sell products themselves, they inherit the financial reporting obligation.
- Group Purchasing Organizations (GPOs): Companies that buy or negotiate purchases for healthcare providers, such as hospitals or practices, must disclose ownership interests and report payments made to physicians or teaching hospitals.
- Foreign manufacturers: Firms outside the U.S. with products reimbursed by federal healthcare programs are also included when those products are sold in the U.S.
The reach of the law is extensive. This breadth ensures that most financial interactions between life sciences companies and healthcare providers are captured, regardless of corporate structure or geography.
What information must be tracked and reported for compliance under the law?
Compliance with the Sunshine Act is carried out by life sciences manufacturers and group purchasing organizations. As a finance leader, you carry the responsibility to ensure that every transfer of value to physicians and teaching hospitals meets CMS requirements.
The obligation is placed on your organization, not on providers, which makes accurate tracking across departments a core part of maintaining compliance.
Payments to physicians and teaching hospitals
Direct payments cover cash, checks, electronic transfers, or other monetary compensation. These payments can relate to a wide range of activities such as consulting, research participation, or general services. For you, this means every dollar paid directly to a physician or teaching hospital must be captured in a structured way.
Ownership and investment interests
You must disclose ownership or investment stakes held by physicians in your company or in related group purchasing organizations. This requirement ensures visibility into potential conflicts of interest.
For finance teams, it involves maintaining accurate records of equity arrangements, profit-sharing agreements, or other financial stakes that extend beyond service payments.
Research funding and clinical trial support
Research-related payments often represent large amounts and complex structures. This includes grants for clinical studies, investigator fees, or support provided to research institutions. These payments often represent significant amounts, with CMS data showing over $8.52 billion in research-related payments in 2024.
Tracking these payments requires coordination between finance, legal, and research teams to ensure that both direct and indirect costs are accounted for in the final report.
Consulting fees, honoraria, and speaking engagements
Healthcare providers are often paid for their expertise through advisory boards, speaker programs, or training sessions. In 2024, this category was the largest share of General Payments, accounting for $1.34B — 40% of all dollars reported — across over 500K transactions. These payments are reportable because they reflect direct financial relationships that can influence medical practice. For you, this means tracking not only the fee itself but also related costs such as travel or accommodations tied to the engagement.
Meals, travel, and lodging
Even routine expenses such as a working lunch or reimbursed travel for a conference must be disclosed. In 2024 alone, meals, travel, and lodging accounted for $615M of spend — just 18% of the $3.33B in General Payments — but represented an outsized 95.8% of all transactions reported.
This imbalance makes them especially burdensome: They dominate compliance workloads by volume despite representing a small share of total dollars. As a result, they are challenging not only for Finance teams to manage but also for Medical Affairs teams to stay on top of. Automation is often essential to link these small but frequent transactions to the correct provider and ensure nothing slips through the cracks.
Educational materials, equipment, and supplies
Items intended for training or clinical use, such as textbooks, demonstration devices, or sample supplies, are considered reportable transfers of value. While these may appear low in dollar value, they form a large share of the total number of records CMS receives each year. For compliance, you need clear categorization to distinguish these items from general business expenses.
Charitable contributions and grants
Donations to nonprofits or grants provided at the request of a physician or teaching hospital must also be included. These transactions can blur the line between philanthropy and influence, which is why regulators require them to be disclosed. In 2024, this category represented a small fraction of General Payments, which is about $125.9M in total spend across fewer than 10K transactions. Tracking them still requires clear documentation of both purpose and recipient to ensure transparency.
Royalties and licensing fees
Payments made to physicians for intellectual property rights, patents, or licensing agreements are often high-value transactions. In 2024, these payments totaled $853M — 26% of all General Payments reported with an average transaction size of $50.6K. These reflect collaborations in product development and must be captured with precise details. For finance leaders, this means working closely with legal and R&D teams to make sure intellectual property agreements are fully reported.
Is manual Sunshine Act compliance challenging for finance teams?
Staying compliant with the Sunshine Act is harder when reporting relies on manual processes. The law demands accuracy, completeness, and timeliness, but manual systems often fall short.
- Fragmented data sources: Spend data is scattered across cards, accounts payable, procurement, research, and charitable contributions. Each source records information differently. Without a central system, you end up reconciling mismatched formats, correcting duplicate entries, and filling gaps manually.
- High transaction volume: CMS received more than 16 million payment records. Each record required details like the recipient’s name, the amount, the date, and the type of payment. When you manage this volume through spreadsheets, small mistakes quickly compound.
- Cross-department involvement: Sunshine Act data rarely live in finance alone. Compliance teams monitor regulatory rules, research teams track clinical trial payments, and procurement manages vendor interactions. Without consistent workflows, records are interpreted differently, making it harder to prove compliance alignment across the organization.
- Changing CMS requirements: Templates, definitions, and validation rules evolve regularly. A manual approach makes it harder to adjust, creating compliance gaps that may only surface during audits.
- Hidden opportunity costs: Life sciences companies spend thousands of hours each year on compliance. Repetitive reconciliation tasks often consume these hours.
The challenge is not only the effort involved. It is that manual processes increase the likelihood of errors, inconsistencies, and delays, which directly put Sunshine Act compliance at risk.
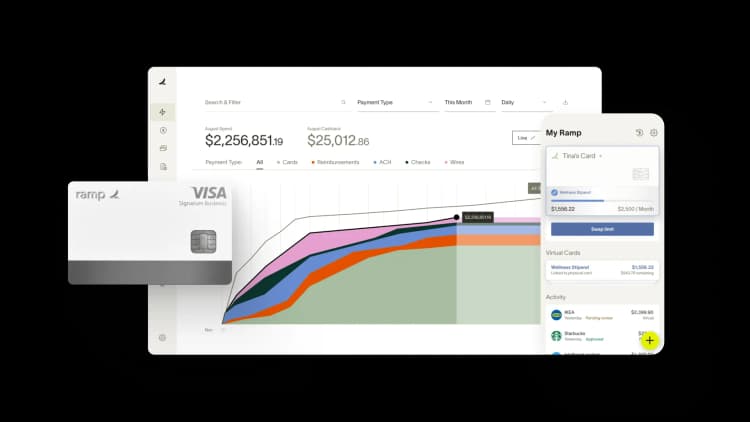
Ramp integrates Sunshine Act compliance into everyday workflows. It tags spend at the point of activity, pulls provider IDs from NPPES, enforces classification rules, and delivers CMS-formatted reporting, all from one platform.
Where automation fits in Sunshine Act compliance workflows
Automation supports Sunshine Act compliance by ensuring that every required payment detail is captured, validated, and organized in real time. Instead of collecting spreadsheets from multiple departments, data flows directly from financial and research systems into one platform.
Each transaction is categorized, matched to the correct provider, and checked against CMS rules. The result is a record that is accurate, consistent, and ready for audits.
Core function | How automation works | Compliance value for teams |
|---|---|---|
Data aggregation | Connects cards, accounts payable, procurement, and research systems into one platform | Ensures all reportable spend is captured without gaps across departments |
Transaction categorization | Applies rules and AI to classify payments into CMS-defined categories | Maintains consistent categorization that aligns with compliance requirements |
Provider matching | Links payments to the official CMS Open Payments database of physicians and hospitals | Reduces misreporting by improving accuracy when providers have similar names |
Audit trail creation | Stores payment records with documentation, timestamps, and validation logs | Builds a complete record that supports CMS audits and internal reviews |
Regulatory updates | Applies new CMS templates, fields, and validation rules automatically | Keeps reports aligned with the latest compliance standards |
Policy enforcement | Embeds company-level rules for allowable spend and disclosure thresholds | Flags transactions that could breach compliance policies before submission |
Workflow automation | Routes payment data through approval chains and compliance reviews digitally | Strengthens oversight by ensuring all payments pass compliance checks |
Error detection | Identifies missing fields, duplicate entries, and outlier transactions early | Lowers compliance risk by preventing corrections during CMS review |
Dashboards and reporting | Provides real-time views for finance, compliance, and leadership teams | Creates visibility into compliance status and readiness throughout the year |
Final submission readiness | Generates reports in the exact CMS Open Payments format | Delivers accurate submissions that reduce the chance of CMS rejection |
Which expenses benefit most from compliance automation
Not every transaction has the same impact on Sunshine Act compliance. Some expenses create risk because of their high volume, while others involve complex agreements or flow across multiple systems.
Manual tracking often leaves gaps that undermine compliance. Automation strengthens oversight in the areas where errors are most common, giving you complete and accurate data before submission.
High-volume routine expenses
Meals, small gifts, and routine interactions with healthcare providers generate thousands of records each year. Each transaction requires provider names, dates, payment amounts, and context.
When you track them manually, it is easy to miss or misclassify details. Incomplete records make your compliance submission vulnerable to errors. Automation captures these expenses directly from cards or expense reports and links them to the correct reporting category. This ensures a full record of high-volume transactions.
Travel and lodging transactions
Airfare, hotel stays, ground transportation, and conference packages often create multiple receipts for a single event. Manually splitting and linking these charges to the right provider leaves room for inconsistencies.
Automation improves compliance by pulling travel spend into one system and then matching each charge to the right provider. It also groups related costs into a single record, reducing the risk of duplicate entries or missing details.
Sana Benefits, for example, used Ramp to reduce out-of-policy travel expenses by 10% reduction. This shows how automated tracking not only improves compliance but also strengthens cost management.
Research and clinical trial funding
Research payments are among the largest transfers of value and involve multiple stakeholders. Grants, investigator fees, and study-related costs must all tie back to protocols and provider records.
Without automation, consolidating this data accurately is difficult and exposes your organization to compliance gaps. Automated systems link direct and indirect research costs to the correct contracts and providers, creating a clear audit trail that supports compliance requirements.
Recurring vendor or consultant payments
Payments for consulting, advisory boards, or contracted services often repeat monthly or quarterly. Manual processes risk inconsistent categorization across vendor reporting periods, which can create compliance discrepancies.
Automation increases reliability by recognizing recurring patterns and applying consistent categorization rules. Each payment is matched to the correct provider and reporting category without relying on manual input.
Out-of-policy or unusual transactions
One-time grants, large non-routine transfers, or expenses flagged during reviews are more likely to be misclassified when tracked by hand. These outliers present heightened compliance risk because they do not fit standard categories.
Automation applies pre-set rules, flags anomalies, and routes them for review before submission. This reduces corrections and strengthens the completeness of your compliance record.
What makes automation the foundation for Sunshine Act compliance?
Automation supports Sunshine Act compliance by capturing every transaction at the point of spend and aligning it with CMS requirements. Instead of piecing data together at the end of the year, you maintain a continuous record that is accurate and complete.
The strength of automation is its consistency. Systems apply the same rules across meals, research payments, travel, and consulting fees, which creates uniform compliance practices across departments and a single reliable source of truth.
Compliance also benefits from greater transparency. Finance, compliance, and leadership teams work from the same real-time data, which reduces gaps and builds confidence that reporting meets regulatory expectations.
Where Ramp fits in your Sunshine Act compliance process
Ramp serves as a compliance-first expense platform that helps you meet Sunshine Act requirements with accuracy and consistency. Each payment captured through Ramp is enriched with the necessary details and mapped to CMS-defined categories. Instead of reconciling data from separate systems, you maintain a single, complete record covering cards, bills, procurement, and reimbursements.
The platform automates compliance workflows by tracking physician payments, categorizing spend in real time, and linking each transfer of value to the correct provider. This reduces the risk of errors and ensures your data meets regulatory expectations.
Ramp also produces audit-ready compliance reports without extra formatting. For finance leaders in healthcare and biotech, this shifts Sunshine Act compliance from a manual burden into a continuous process built into daily operations.

FAQs
CMS requires manufacturers and group purchasing organizations to remain compliant by submitting all transfers of value from the previous calendar year by March 31. Physicians and teaching hospitals have a 45-day period to review and dispute data, after which CMS finalizes the records. Public release typically occurs in June, making timely compliance essential.
CMS exempts transfers of value under $13.46, unless the total given to a single physician exceeds $134.54 in a calendar year. Once the aggregate threshold is crossed, every transfer must be reported. These thresholds adjust annually, so compliance requires tracking both individual and cumulative spend.
Indirect payments arise when value is transferred to a provider on behalf of a manufacturer or at its direction, even through third parties. CMS requires these to be disclosed, making it necessary to trace and attribute the payment to the ultimate recipient to remain compliant.
Since 2021, the definition of covered recipients expanded to include nurse practitioners, physician assistants, clinical nurse specialists, certified registered nurse anesthetists, and certified nurse midwives. Compliance now extends to a much larger group of healthcare professionals.
If errors are identified after submission, manufacturers and GPOs must update their records through the CMS Open Payments portal. Corrections replace the original entries and are flagged publicly to show that a change was made. Updates can be submitted at any time, but compliance depends on maintaining accuracy even after publication.
“In the public sector, every hour and every dollar belongs to the taxpayer. We can't afford to waste either. Ramp ensures we don't.”
Carly Ching
Finance Specialist, City of Ketchum

“Ramp gives us one structured intake, one set of guardrails, and clean data end‑to‑end— that’s how we save 20 hours/month and buy back days at close.”
David Eckstein
CFO, Vanta

“Ramp is the only vendor that can service all of our employees across the globe in one unified system. They handle multiple currencies seamlessly, integrate with all of our accounting systems, and thanks to their customizable card and policy controls, we're compliant worldwide. ”
Brandon Zell
Chief Accounting Officer, Notion

“When our teams need something, they usually need it right away. The more time we can save doing all those tedious tasks, the more time we can dedicate to supporting our student-athletes.”
Sarah Harris
Secretary, The University of Tennessee Athletics Foundation, Inc.

“Ramp had everything we were looking for, and even things we weren't looking for. The policy aspects, that's something I never even dreamed of that a purchasing card program could handle.”
Doug Volesky
Director of Finance, City of Mount Vernon

“Switching from Brex to Ramp wasn't just a platform swap—it was a strategic upgrade that aligned with our mission to be agile, efficient, and financially savvy.”
Lily Liu
CEO, Piñata

“With Ramp, everything lives in one place. You can click into a vendor and see every transaction, invoice, and contract. That didn't exist in Zip. It's made approvals much faster because decision-makers aren't chasing down information—they have it all at their fingertips.”
Ryan Williams
Manager, Contract and Vendor Management, Advisor360°

“The ability to create flexible parameters, such as allowing bookings up to 25% above market rate, has been really good for us. Plus, having all the information within the same platform is really valuable.”
Caroline Hill
Assistant Controller, Sana Benefits


